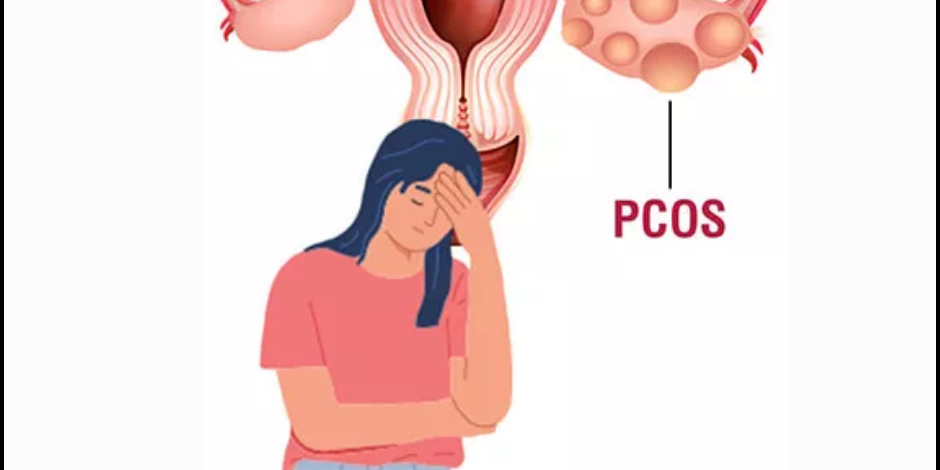
Polycystic Ovary Syndrome, commonly known as PCOS, is a prevalent hormonal disorder that affects people assigned female at birth. PCOS is a medical condition characterized by an imbalance of hormones in individuals with ovaries. It is a complex condition with various manifestations and impacts on reproductive, metabolic, and overall health. One of the key features of PCOS is the presence of small, fluid-filled sacs or cysts in the ovaries, which can interfere with normal ovulation. This disruption in the menstrual cycle can lead to a range of symptoms and complications.
Who can get PCOS?
PCOS can affect people of all ethnicities and backgrounds, and it is estimated to affect approximately 5-10% of people assigned female at birth during their reproductive years. It often becomes noticeable during adolescence, but it can also be diagnosed later in life.
What are the Types of PCOS?
PCOS is not a one-size-fits-all condition. There are different types of PCOS, and individuals may experience varying combinations of symptoms. The main types include:
1. Classic PCOS: This is the most common type, characterized by irregular periods, cysts on the ovaries, and high levels of androgens (male hormones).
2. Non-Classic PCOS: Some individuals may have PCOS-like symptoms without the typical cysts on their ovaries.
3. Lean PCOS: In this subtype, individuals with a lower body mass index (BMI) may still experience PCOS symptoms, which can make diagnosis more challenging.
What are the Causes of PCOS?
The exact cause of PCOS is not fully understood, but it is believed to be multifactorial, involving both genetic and environmental factors. Some contributing factors and risk factors include:
1. Genetics: PCOS tends to run in families, suggesting a genetic component.
2. Insulin Resistance: Many individuals with PCOS have insulin resistance, which can lead to increased insulin levels and affect hormone regulation.
3. Hormonal Imbalance: Elevated levels of androgens, such as testosterone, can disrupt the normal menstrual cycle and contribute to PCOS symptoms.
4. Inflammation: Chronic low-grade inflammation may also play a role in PCOS development.
What are the Symptoms of PCOS?
PCOS can manifest in a variety of ways, and not all individuals will experience the same symptoms. Common signs and symptoms of PCOS include:
1. Irregular or absent menstrual periods
2. Excessive hair growth (hirsutism)
3. Acne and oily skin
4. Weight gain or difficulty losing weight
5. Hair loss or thinning on the scalp
6. Pelvic pain
7. Mood changes, including depression and anxiety
It’s essential to note that PCOS symptoms can extend beyond reproductive health, impacting metabolic and cardiovascular health as well.
How is PCOS Diagnosed?
Diagnosing PCOS requires a comprehensive evaluation by a healthcare professional. The diagnostic process typically includes:
1. Medical History: Your healthcare provider will inquire about your menstrual history, symptoms, and family history of PCOS or related conditions.
2. Physical Examination: A physical examination may be conducted to assess signs of PCOS, such as hirsutism or acne.
3. Blood Tests: Blood tests will measure hormone levels, including testosterone and insulin. Elevated levels may indicate PCOS.
4. Pelvic Ultrasound: An ultrasound may be performed to visualize the ovaries and check for the presence of cysts.
To be diagnosed with PCOS, individuals typically need to meet specific criteria, such as irregular periods, elevated androgen levels, and exclusion of other conditions that could mimic PCOS symptoms.
How is PCOS Treated?
The management of PCOS primarily focuses on addressing individual symptoms and reducing long-term health risks. PCOS Treatment options include:
1. Lifestyle Modifications: Healthy lifestyle changes, including a balanced diet, regular exercise, and weight management, can help improve insulin sensitivity and hormone balance.
2. Medications: Depending on the symptoms, healthcare providers may prescribe medications like birth control pills to regulate periods, anti-androgen medications to address hirsutism and acne, or metformin to improve insulin sensitivity.
3. Fertility Treatments: For those trying to conceive, fertility treatments like ovulation induction or in vitro fertilization (IVF) may be recommended.
4. Surgery: In rare cases, surgery may be necessary to remove cysts or address other complications.
If you suspect you have PCOS or have been diagnosed with it, consulting a healthcare professional or fertility expert is crucial to developing an effective management strategy tailored to your specific needs.